Major surgery is always a daunting prospect, no matter the specifics of the procedure. However, when it comes to cosmetic surgeries such as a boob job or a c-section, the risks are generally considered to be lower due to the fact that they do not involve major organs. These types of surgeries are often classified as routine, despite the fact that they are still invasive procedures that require careful post-operative care.
A boob job, also known as breast augmentation, involves the insertion of implants to increase the size or alter the shape of the breasts. While the procedure itself may not be as extensive as other surgeries, such as open heart surgery or a kidney transplant, it still comes with its own set of risks and challenges. One of the most common complaints from patients who have undergone a boob job is the restriction of movement in the torso area. This can make simple tasks such as getting out of bed or picking up objects difficult and painful. In addition, the recovery process can be quite intense, with many patients reporting feeling like death for the first two weeks post-surgery. Keeping up with pain medication is crucial during this time to help manage discomfort and promote healing.
On the other hand, a c-section is a surgical procedure in which a baby is delivered through an incision in the mother’s abdomen and uterus. While the c-section procedure is often necessary for medical reasons, such as complications during labor or the baby being in distress, it is still considered to be a major surgery. The recovery process for a c-section is similar to that of a boob job, with patients typically experiencing discomfort and limited mobility for the first few weeks post-surgery. Pain management is also key during this time to help the body heal properly.
In conclusion, while both a boob job and a c-section are considered major surgeries, they do not involve major organs and are therefore classified as routine and low risk. However, the recovery process for both procedures can be challenging and painful, requiring careful attention to pain management and post-operative care. It is important for patients considering either of these surgeries to be aware of the potential risks and challenges involved, and to work closely with their healthcare providers to ensure a smooth and successful recovery.
| Procedure | Description | Recovery Time |
|——————-|—————————————————————————————————————————————————————————|————————————————–|
| Boob Job | Breast augmentation surgery involving the insertion of implants to increase breast size or alter shape. | 2 weeks of restricted movement, intense discomfort |
| C-Section | Surgical delivery of a baby through an incision in the mother’s abdomen and uterus. | Similar recovery time to boob job, limited mobility|
In this article we will discuss about Risks of breastfeeding with implants and what hurts more c section or breast augmentation
Breast Augmentation Vs C Section
BREAST AUGMENTATION
Overview
It involves placing breast implants under breast tissue or chest muscles.
For others, it’s part of rebuilding the breast for various conditions.
Make sure you understand what surgery involves, including possible risks, complications and follow-up care.
Why it’s done
Breast augmentation might help you:
- Enhance your appearance if you think your breasts are small or that one is smaller than the other and this impacts how you dress or the type of bra needed to help with the asymmetry
- Adjust for a reduction in the size of your breasts after pregnancy or significant weight loss
- Correct uneven breasts after breast surgery for other conditions
- Improve your self-confidence
Discuss your goals with your plastic surgeon so that you can be realistic about what breast augmentation can do for you.
Risks
Breast augmentation poses various risks, including:
- Scar tissue that distorts the shape of the breast implant (capsular contracture)
- Breast pain
- Infection
- Changes in nipple and breast sensation
- Implant position changes
- Implant leakage or rupture
Correcting these complications might require more surgery, to either remove or replace the implants.
Breast implant-associated anaplastic large cell lymphoma
The condition is known as breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). The FDA believes that women with breast implants that have textured surfaces have a very low but increased risk of developing BIA-ALCL. However, that doesn’t mean that these implants cause BIA-ALCL. Further research is needed to understand the relationship between the condition and breast implants.
Breast implant illness
Systemic symptoms ― sometimes called breast implant illness ― may be associated with breast implants. The exact relationship of these symptoms to breast implants is not clearly understood. Reported signs and symptoms include fatigue, memory loss, skin rash, trouble concentrating and thinking clearly, and joint pain. Removal of the breast implants may reverse the symptoms. Research to determine the link and the cause is ongoing. Talk to your plastic surgeon if you have breast implants and experience any of these signs and symptoms.
If you notice any changes to your breasts or implants, talk to your doctor. Ongoing follow-up visits and appropriate screening tests can detect and address possible complications related to breast augmentation surgery.
How you prepare
You’ll consult with a plastic surgeon about your preferences for size, feel and appearance of your breasts. The surgeon will describe specific types of implants — smooth or textured, round or shaped like a teardrop, saline or silicone — as well as options for surgical techniques.
Carefully review written information, such as the patient information from the manufacturer of the implant you’ll be getting, and keep copies for your records.
- Implant rupture is a possibility. Also, your breasts will continue to age, and factors such as weight gain or weight loss might change the way your breasts look. These issues will likely lead to more surgery.
- Mammograms might be more complicated. If you have breast implants, in addition to routine mammograms, you’ll need additional, specialized views.
- Breast implants might hamper breast-feeding. Some women are able to successfully breast-feed after breast augmentation. For others, however, breast-feeding is a challenge.
- Insurance doesn’t cover breast implants. Unless it’s medically necessary — such as after a mastectomy for breast cancer — breast augmentation isn’t covered by insurance. Be prepared to handle the expenses, including related surgeries or future imaging tests.
- You might need additional surgery after breast implant removal. If you decide to have your implants removed, you might need a breast lift or other corrective surgery to help restore your breasts’ appearance.
- Screening for silicone implant rupture is recommended. The FDA recommends routine monitoring with a breast MRI five to six years after placement to screen for silicone breast implant rupture. Then, a breast MRI is recommended every two to three years. An ultrasound may be an alternative screening method — unless you have symptoms. Talk to your plastic surgeon about the specific type of imaging needed for routine monitoring of your implants.
You might need a baseline mammogram before your surgery. Your doctor might adjust certain medications before the surgery as well. For example, it’s important to avoid aspirin or other medications that can increase bleeding.
If you smoke, your surgeon will ask you to stop smoking for a time ― about four to six weeks ― before and after the surgery.
Arrange for someone to drive you home after the surgery and to stay with you for at least the first night.
What you can expect
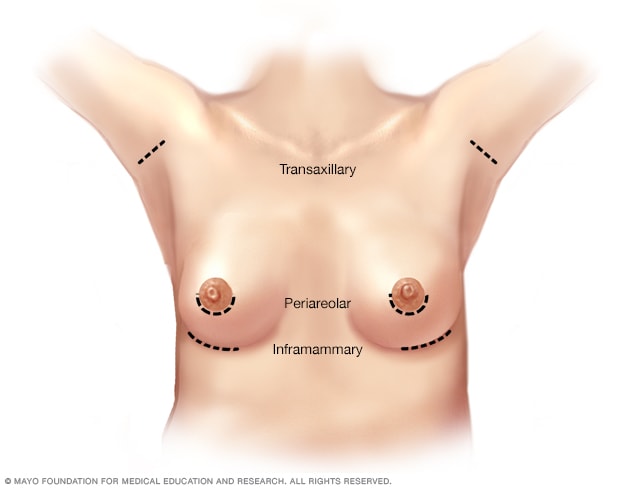 Breast augmentation incision sitesOpen pop-up dialog box
Breast augmentation incision sitesOpen pop-up dialog box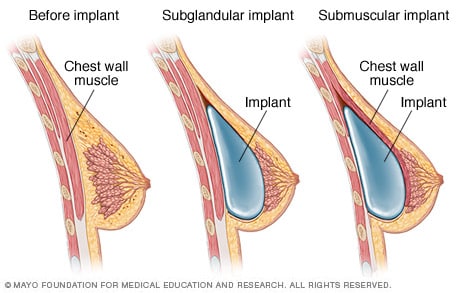 Placement of breast implantsOpen pop-up dialog box
Placement of breast implantsOpen pop-up dialog box
Breast augmentation can be done in a surgical center or hospital outpatient facility. You’ll probably go home the same day. The procedure rarely requires a hospital stay.
Sometimes, breast augmentation is done during local anesthesia — you’re awake and your breast area is numbed. Often, though, breast augmentation is done during general anesthesia, in which you’re asleep for the surgery. Your plastic surgeon will review different anesthesia options with you.
During the procedure
To insert the breast implant, your plastic surgeon will make a single cut (incision) in one of three places:
- The crease under your breast (inframammary)
- Under your arm (axillary)
- Around your nipple (periareolar)
After making an incision, the surgeon will separate your breast tissue from the muscles and connective tissue of your chest. This creates a pocket either behind or in front of the outermost muscle of the chest wall (pectoral muscle). The surgeon will insert the implant into this pocket and center it behind your nipple.
Saline implants are inserted empty and then filled with sterile salt water once they’re in place. Silicone implants are pre-filled with silicone gel.
When the implant is in place, the surgeon will close the incision — typically with stitches (sutures) — and bandage it with skin adhesive and surgical tape.
After the procedure
Soreness and swelling are likely for a few weeks after surgery. Bruising is possible, too. Expect scars to fade over time but not disappear completely.
While you’re healing, it might help to wear a compression bandage or sports bra for extra support and positioning of the breast implants. Your surgeon might prescribe pain medication as well.
Follow your surgeon’s instructions about returning to regular activities. Avoid strenuous activities — anything that could raise your pulse or blood pressure — for at least two weeks. While you’re healing, remember that your breasts will be sensitive to physical contact or jarring movements.
If your surgeon used sutures that don’t absorb on their own or placed drainage tubes near your breasts, you’ll need a follow-up appointment for removal.
If you notice warmth and redness in your breast or you have a fever, you might have an infection.
Results
The surgery might improve your body image and self-esteem. But keep your expectations realistic, and don’t expect perfection.
Also, your breasts will continue to age after augmentation. Weight gain or weight loss might change the way your breasts look, too. If you become dissatisfied with the appearance of your breasts, you might need more surgery to correct these issues.
C-section
Overview
A C-section might be planned ahead of time if you develop pregnancy complications or you’ve had a previous C-section and aren’t considering a vaginal birth after cesarean (VBAC). Often, however, the need for a first-time C-section doesn’t become obvious until labor is underway.
Some women request C-sections with their first babies — to avoid labor or the possible complications of vaginal birth or to take advantage of the convenience of a planned delivery. However, this is discouraged if you plan on having several children. Women who have multiple C-sections are at increased risk of placental problems as well as heavy bleeding, which might require surgical removal of the uterus (hysterectomy). If you’re considering a planned C-section for your first delivery, work with your health care provider to make the best decision for you and your baby.
Risks
Like other types of major surgery, C-sections also carry risks.
Risks to your baby include:
- Breathing problems. Babies born by scheduled C-section are more likely to develop transient tachypnea — a breathing problem marked by abnormally fast breathing during the first few days after birth.
- Surgical injury. Although rare, accidental nicks to the baby’s skin can occur during surgery.
Risks to you include:
- Infection. After a C-section, you might be at risk of developing an infection of the lining of the uterus (endometritis).
- Postpartum hemorrhage. A C-section might cause heavy bleeding during and after delivery.
- Reactions to anesthesia. Adverse reactions to any type of anesthesia are possible.
- Blood clots. A C-section might increase your risk of developing a blood clot inside a deep vein, especially in the legs or pelvic organs (deep vein thrombosis). If a blood clot travels to your lungs and blocks blood flow (pulmonary embolism), the damage can be life-threatening.
- Wound infection. Depending on your risk factors and whether you needed an emergency C-section, you might be at increased risk of an incision infection.
- Surgical injury. Although rare, surgical injuries to the bladder or bowel can occur during a C-section. If there is a surgical injury during your C-section, additional surgery might be needed.
- Increased risks during future pregnancies. After a C-section, you face a higher risk of potentially serious complications in a subsequent pregnancy than you would after a vaginal delivery. The more C-sections you have, the higher your risks of placenta previa and a condition in which the placenta becomes abnormally attached to the wall of the uterus (placenta accreta). The risk of your uterus tearing open along the scar line from a prior C-section (uterine rupture) is also higher if you attempt a VBAC.
How you prepare
If your C-section is scheduled in advance, your health care provider might suggest talking with an anesthesiologist about any possible medical conditions that would increase your risk of anesthesia complications.
Your health care provider might also recommend certain blood tests before your C-section. These tests will provide information about your blood type and your level of hemoglobin, the main component of red blood cells. These details will be helpful to your health care team in the unlikely event that you need a blood transfusion during the C-section.
Even if you’re planning a vaginal birth, it’s important to prepare for the unexpected. Discuss the possibility of a C-section with your health care provider well before your due date. Ask questions, share your concerns and review the circumstances that might make a C-section the best option. In an emergency, your health care provider might not have time to explain the procedure or answer your questions in detail.
After a C-section, you’ll need time to rest and recover. Consider recruiting help ahead of time for the weeks after the birth of your baby.
If you don’t plan to deliver any more children, you might talk to your health care provider about long-acting reversible birth control or permanent birth control.
What you can expect
Before the procedure
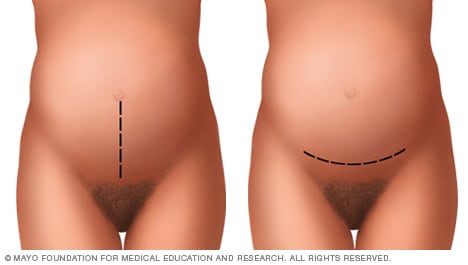 Abdominal incisions used during C-sectionsOpen pop-up dialog box
Abdominal incisions used during C-sectionsOpen pop-up dialog box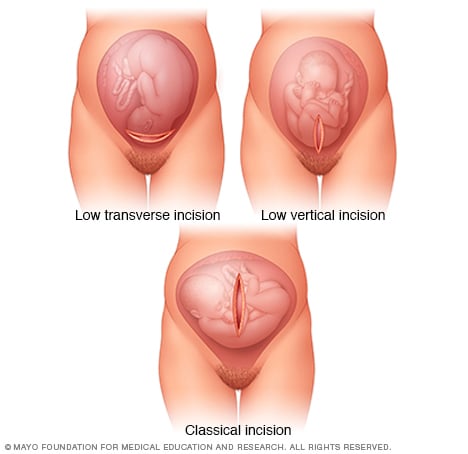 Uterine incisions used during C-sectionsOpen pop-up dialog box
Uterine incisions used during C-sectionsOpen pop-up dialog box
While the process can vary, depending on why the procedure is being done, most C-sections involve these steps:
- At home. Your health care provider might ask you to shower with an antiseptic soap the night before and the morning of your C-section. Don’t shave your pubic hair within 24 hours of your C-section. This can increase the risk of a surgical site infection. If your pubic hair needs to be removed, it will be trimmed by the surgical staff just before surgery.
- At the hospital. Your abdomen will be cleansed. A tube (catheter) will likely be placed into your bladder to collect urine. Intravenous (IV) lines will be placed in a vein in your hand or arm to provide fluid and medication.
- Anesthesia. Most C-sections are done under regional anesthesia, which numbs only the lower part of your body — allowing you to remain awake during the procedure. Common choices include a spinal block and an epidural block. In an emergency, general anesthesia is sometimes needed. With general anesthesia, you won’t be able to see, feel or hear anything during the birth.
During the procedure
While the process can vary, depending on why the procedure is being done, most C-sections involve these steps:
- At home. Your health care provider might ask you to shower with an antiseptic soap the night before and the morning of your C-section. Don’t shave your pubic hair within 24 hours of your C-section. This can increase the risk of a surgical site infection. If your pubic hair needs to be removed, it will be trimmed by the surgical staff just before surgery.
- At the hospital. Your abdomen will be cleansed. A tube (catheter) will likely be placed into your bladder to collect urine. Intravenous (IV) lines will be placed in a vein in your hand or arm to provide fluid and medication.
- Anesthesia. Most C-sections are done under regional anesthesia, which numbs only the lower part of your body — allowing you to remain awake during the procedure. Common choices include a spinal block and an epidural block. In an emergency, general anesthesia is sometimes needed. With general anesthesia, you won’t be able to see, feel or hear anything during the birth.
After the procedure
After a C-section, you’ll probably stay in the hospital for a few days. Your health care provider will discuss pain relief options with you.
Once the effects of your anesthesia begin to fade, you’ll be encouraged to drink plenty of fluids and walk. This helps prevent constipation and deep vein thrombosis. Your health care team will monitor your incision for signs of infection. If you had a bladder catheter, it will likely be removed as soon as possible.
Your health care team will select medications for your post-surgical pain with breast-feeding in mind.
When you go home
During the C-section recovery process, discomfort and fatigue are common. To promote healing:
- Take it easy. Rest when possible. Try to keep everything that you and your baby might need within reach. For the first few weeks, avoid lifting anything heavier than your baby. Also, avoid lifting from a squatting position.
- Seek pain relief. To soothe incision soreness, your health care provider might recommend a heating pad, ibuprofen (Advil, Motrin, others), acetaminophen (Tylenol, others) or other medications to relieve pain. Most pain relief medications are safe for women who are breast-feeding.
- Avoid sex. To prevent infection, avoid sex for six weeks after your C-section.
You might also consider not driving until you are able to comfortably apply brakes and twist to check blind spots without the help of pain medication. This might take one to two weeks.
Check your C-section incision for signs of infection. Pay attention to any signs or symptoms you experience. Contact your health care provider if:
- Your incision is red, swollen or leaking discharge
- You have a fever
- You have heavy bleeding
- You have worsening pain
If you experience severe mood swings, loss of appetite, overwhelming fatigue and lack of joy in life shortly after childbirth, you might have postpartum depression. Within 12 weeks after delivery, see your health care provider for a comprehensive postpartum evaluation. During this appointment your health care provider will check your mood and emotional well-being, discuss contraception and birth spacing, review information about infant care and feeding, talk about your sleep habits and issues related to fatigue and do a physical exam. This might include a check of your abdomen, vagina, cervix and uterus to make sure you’re healing well. In some cases, you might have the checkup earlier so that your health care provider can examine your C-section incision. Use this visit to ask questions about your recovery and caring for your baby.
What Hurts More C Section Or Breast Augmentation
Surgery is a big decision. Patients have all kinds of questions for Dr. Bernard Beldholm when they come in for a consultation. Doctor Bernard always makes time to answer all questions. If you are still researching tummy tuck surgery, he wants to put your fears to rest. Knowing what to expect walking into surgery can be a huge relief.
So, is a tummy tuck similar to a c-section in terms of pain? That’s something many women want to know.
While patients have different experiences, most plastic surgeons would agree that a cesarean section is more painful than most tummy tucks. A tummy tuck without muscle repair just involves the top layers of the tummy. A c-section is also a major surgery, but the healing time is longer. We’re talking months for a c-section compared to 6-8 weeks for a tummy tuck. A c-section goes deeper into the abdominal cavity than a tummy tuck without muscle repair.
Risks Of Breastfeeding With Implants
Research on the Safety of Silicone Breast Implants in Mothers and InfantsRecently, there have been concerns regarding the safety of silicone breast implants in mothers who are breastfeeding. However, limited research has been conducted in this area, making it challenging to draw definitive conclusions. Despite the lack of extensive studies, no recent reports have indicated any clinical problems in infants of mothers with silicone breast implants.Studies on the potential risks of silicone breast implants during breastfeeding have been limited, with most research focusing on the safety of silicone implants in general. The FDA has approved the use of silicone breast implants for breast augmentation and reconstruction, citing them as safe and effective. However, the agency recommends regular monitoring for potential complications such as rupture or leakage.It is important to note that silicone breast implants are considered safe for both the mother and baby during breastfeeding. Silicone is an inert material that does not pass into breast milk, meaning it is unlikely to be ingested by the infant. Additionally, silicone breast implants are encased in a silicone shell, which further reduces the risk of leakage or migration of silicone material.Although research on the safety of silicone breast implants during breastfeeding is limited, healthcare providers should still monitor mothers with implants closely for any signs of complications. It is essential for mothers with breast implants to inform their healthcare providers about their implants before breastfeeding to ensure proper monitoring and support.
| Key PointsSilicone breast implants are considered safe for mothers and infants during breastfeeding.Research on the safety of silicone breast implants during breastfeeding is limited.No recent reports have indicated any clinical problems in infants of mothers with silicone breast implants. |
|---|
Overall, while more research is needed to fully understand the potential risks of silicone breast implants during breastfeeding, current evidence suggests that these implants are safe for both mothers and infants. Healthcare providers should continue to monitor and support mothers with implants to ensure their health and well-being during breastfeeding.
Can a mother breastfeed after breast or nipple surgery?
Tips for helping mothers who have had breast surgery
Prenatal support:
- Talk with mothers who have had breast surgery about the type of surgery, placement of incisions, and underlying reasons for the surgery to understand the potential for reduced milk production.
- Examine mothers’ breasts to identify possible insufficient glandular tissue and provide anticipatory guidance for breastfeeding support.
Postpartum support:
- Closely monitor infants of mothers who have had breast surgery to be sure that the infant receives optimal nutrition for growth.
- When mothers present with insufficient milk production postpartum, inquire about prior breast surgery as part of your assessment.
- Refer to an International Board Certified Lactation Consultant (IBCLC) to teach mothers who have had breast surgery how to stimulate production and/or how to supplement with pasteurized donor human milk or formula.
- Ensure that mothers who have had breast surgery and encounter breastfeeding challenges receive appropriate emotional support.
Usually. Most mothers who have had breast or nipple surgery are able to produce some milk, but not all of these mothers will be able to produce a full milk supply for their infants. Having a full milk supply is not necessary for a successful breastfeeding experience because it is possible to supplement in a way that supports breastfeeding.
Breast Augmentation, lift, and reduction:
Breast augmentation, lift, and reduction procedures have the potential to affect the nerves and ducts within the breast, thus impacting lactation. Breast implants below the muscle usually affect milk production less than implants above the muscle. Incisions around the areola and surgical techniques that include completely detaching the areolae and nipples are more likely to cause reductions in milk production. Over time, ducts that were severed during surgery may grow back together or form new pathways, and nerves may regain functionality, enabling the mother to produce milk. A scar around the whole areola following breast reduction does not indicate complete detachment because it may have remained connected to tissue containing nerves, ducts, and blood supply. The amount of milk made will depend on the number of connected ducts and functionality of the nerves that enable lactation, as well as other factors apart from the surgery, such as hormones and milk removal. Babies of mothers who have had breast surgery should be carefully monitored for adequate weight gain. Mothers may need support to increase milk production and/or to supplement with pasteurized donor human milk or formula.
Mastectomy:
Women who have been treated for breast cancer with partial or total mastectomy may have reduced capability to breastfeed or produce breast milk. Partial or total mastectomy can result in removal of breast tissue and damage to essential nerves involved in lactation. Women with total mastectomy of one breast should plan for unilateral breastfeeding. Women with partial mastectomy and radiation therapy should expect significantly reduced milk production on the affected side(s). A single breast can produce enough breast milk for healthy infant growth. However, dyads should be followed closely for adequate infant weight gain. Further guidance is outlined in the Academy of Breastfeeding Medicine’s clinical protocol on Breast Cancer and Breastfeeding.
Women may have varied experiences with breastfeeding after breast cancer treatment and may encounter a range of social and psychological challenges. Providers may need to address psychosocial challenges when supporting the infant feeding decisions of women who have had breast cancer.
Hypoplastic breasts:
Some mothers may have had underdeveloped (hypoplastic) breasts prior to having breast surgery. Mammary hypoplasia, or insufficient glandular tissue, is characterized by breasts that appear tubular, widely-spaced, or significantly asymmetrical, leading some women with this condition to seek reconstructive surgery. Mothers who have had hypoplastic breasts may not be able to produce enough milk (primary lactation failure) and will need lactation support to learn how to stimulate production and/or how to supplement with pasteurized donor human milk or formula.
