Breast reconstruction after mastectomy is a complex process that can be very difficult to navigate. It’s important to have all of the information you need up front, so you can make informed choices about your care and decide whether or not breast reconstruction is right for you.
Breast reconstruction is an option for women who have had a mastectomy due to cancer, or for those who have had a prophylactic mastectomy (that is, one without a specific medical reason). This can include women who had breast cancer but whose bodies are otherwise healthy enough to undergo surgery.
The goal of this procedure is to restore what was lost when your breasts were removed: symmetry and function. Breast reconstruction will help you feel more confident in your body and improve your overall quality of life.
In this article, we’ll discuss some of the different types of breast reconstruction options available today: bilateral symmetric flap; unilateral symmetric flap; TRAM flap; DIEP flap; latissimus dorsi flap; DIEP/latissimus dorsi combination flap; transverse rectus abdominis musculocutaneous (TRAM) flap with latissimus dorsi muscle transfer.:
Breast Reconstruction After Mastectomy Diep Flap

The DIEP flap breast reconstruction is today’s most advanced form of breast reconstruction. The procedure uses the patient’s lower abdominal skin and fat to reconstruct a breast after mastectomy but unlike the TRAM flap procedure, preserves all the abdominal muscles.
Benefits of the DIEP flap procedure over implant reconstruction include:
- No foreign objects. Only the patient’s skin and fat are used.
- The reconstructed breast(s) are warm and soft to the touch, not cool like some implant reconstructions.
- Sensory nerve reconstruction can be performed with the DIEP flap (and SIEA flap) to restore sensation after mastectomy.
- The reconstructed breast is permanent. Unlike some implant patients, DIEP patients do not experience increasing breast hardening (capsular contracture) or implant ruptures over time, and rarely need additional surgery once the reconstructive process is complete.
When considering DIEP flap breast reconstruction, a big concern for many patients is post-operative pain. Many patients believe reconstruction with implants is the least painful option since the procedure is less invasive and has a shorter operative time than DIEP flap. However, studies have shown this is not the case.
Although the DIEP flap procedure is more invasive and requires a longer surgery than traditional (subpectoral) tissue expander/implant reconstruction, DIEP flap patients experience less pain for a couple of reasons:
- Minimal muscle trauma. Most implant-based reconstructions involve placing the implant under the chest muscle. This requires releasing and lifting the “pec” muscle off the chest wall to create a pocket for the implant. This is painful and adds to patient recovery.
- For patients who are not candidates for direct-to-implant procedures, tissue expanders are filled over time to stretch the overlying breast tissues. This expansion process can be very uncomfortable for patients when the expander is placed under the muscle.
Healing and recovery after DIEP flap breast reconstruction can be significantly easier than most patients think. With the implementation of ERAS Protocols, most patients experience little discomfort after surgery, require little if any narcotics, and can be discharged from the hospital after 3 days or less.
Here is a quick snapshot of what to expect:
Week 1
First 2-3 days are spent in the hospital to recover. Patients should expect to be walking multiple times the day after surgery and can gradually increase walking time and distance as they feel comfortable. By day 3, most patients can head home.
Week 2
If drains are used they are removed once drain output is low enough. Patients can continue to increase their cardio endurance and begin easing into post-operative range of motion arm exercises. By the end of the second week patients can switch from surgical garments to a bra and panty girdle (be sure to get clearance from your doctor or nurse first).
Week 3-4
Patients should feel more capable of doing things on their own. Patients with low impact desk jobs can return to work.
Week 5-6
Most patients are getting back to their normal routine. By week six there are no restrictions.
The DIEP flap is an excellent alternative to implants for patients seeking to recreate a warm, soft, “natural” breast after mastectomy. ERAS protocols have minimized post-operative discomfort and shortened recovery significantly, further strengthening the DIEP flap’s position as today’s “gold standard” in breast reconstruction.
Breast reconstruction with flap surgery
Overview
Breast reconstruction is a surgical procedure that restores shape to your breast after a mastectomy — surgery that removes your breast to treat or prevent breast cancer. Breast reconstruction with flap surgery involves taking a section of tissue from one area of your body — most often your abdomen — and relocating it to create a new breast mound.
Breast reconstruction with flap surgery is a complex procedure performed by a plastic surgeon. Much of the breast reconstruction using your body’s own tissue can be accomplished at the time of your mastectomy (immediate reconstruction), though sometimes it can be done as a separate procedure later (delayed reconstruction).
Your plastic surgeon may recommend a two-stage procedure. The first stage is to place an implant expander and the second stage is to complete the tissue reconstruction. You’ll likely need another operation to perform nipple reconstruction.
Risks
Breast reconstruction with flap surgery is a major procedure and carries with it the possibility of significant complications, including:
- Changes in breast sensation
- Prolonged time in surgery and under anesthesia
- Extended recovery and healing time
- Poor wound healing
- Fluid collection (seroma)
- Infection
- Bleeding
- Tissue death (necrosis) due to insufficient blood supply
- Loss of sensation at the tissue donor site
- Abdominal wall hernia or weakness
Radiation therapy delivered to the skin and chest wall may pose complications during healing if it’s given after breast reconstruction surgery. Your doctor may recommend waiting until you’re finished with radiation therapy before proceeding with the second stage of the breast reconstruction.
How you prepare
Before a mastectomy, your doctor may recommend that you meet with a plastic surgeon. Consult a plastic surgeon who’s board certified and experienced in breast reconstruction following mastectomy. Ideally, your breast surgeon and the plastic surgeon should work together to develop the best surgical treatment and breast reconstruction strategy in your situation.
Your plastic surgeon will describe your surgical options and may show you photos of women who have had different types of breast reconstruction. Your body type, health status and cancer treatment factor into which type of reconstruction will give you the best result. The plastic surgeon also provides information on anesthesia, where the operation will be performed and what kind of follow-up procedures may be necessary.
Your plastic surgeon may discuss the pros and cons of surgery on your opposite breast, even if it’s healthy, so that it more closely matches the shape and size of your reconstructed breast. Surgery to remove your healthy breast (contralateral prophylactic mastectomy) can double the risk of surgical complications, such as bleeding and infection. Also, there may be less satisfaction with cosmetic outcomes after surgery.
Before surgery, follow your doctor’s instructions on preparing for the procedure. This may include guidelines on eating and drinking, adjusting current medications, and quitting smoking.
What you can expect
Chances are your new breast won’t look exactly like your natural one did. However, the contour of your new breast can usually be restored so that your silhouette looks similar to your silhouette before surgery.
Breast reconstruction with flap surgery is the most complex breast reconstructive option. Your surgeon transfers a section of skin, muscle, fat and blood vessels from one part of your body to your chest to create a new breast mound. In some cases, the skin and tissue need to be augmented with a breast implant to achieve the desired breast size.
Surgical methods
Autologous tissue breast reconstruction uses one of two surgical methods:
- Pedicled flap surgery The surgeon cuts some of the blood vessels to the tissue to be transferred but keeps other blood vessels intact. Tunneling the tissue beneath your skin to your chest area, the surgeon then creates the new breast mound or pocket for the implant.
- Free flap surgery. The surgeon disconnects the tissue completely from its blood supply and reattaches the tissue to new blood vessels near your chest. Because of reattaching blood vessels, free flap surgery typically takes longer than does pedicled flap surgery.
Types of flap surgery
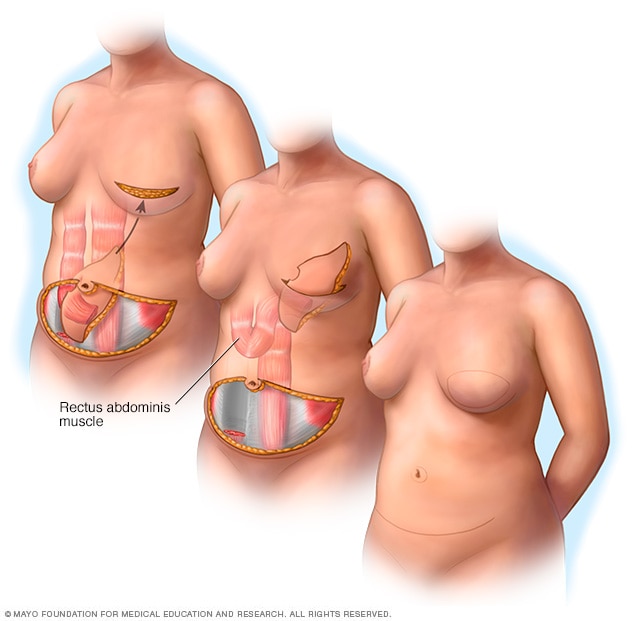 Pedicle TRAM flapOpen pop-up dialog box
Pedicle TRAM flapOpen pop-up dialog box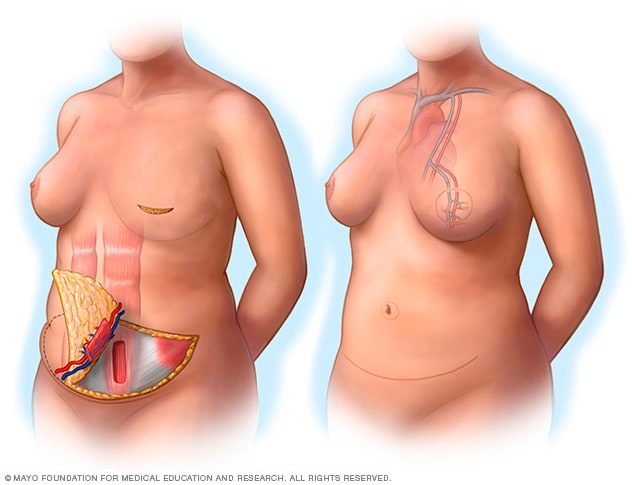 Free TRAM flapOpen pop-up dialog box
Free TRAM flapOpen pop-up dialog box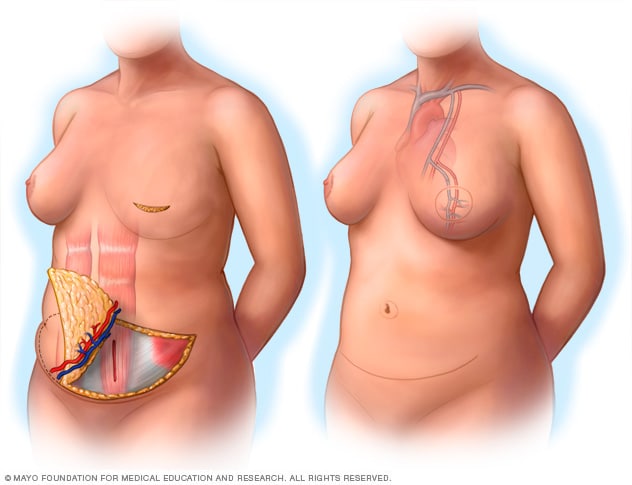 DIEP flapOpen pop-up dialog box
DIEP flapOpen pop-up dialog box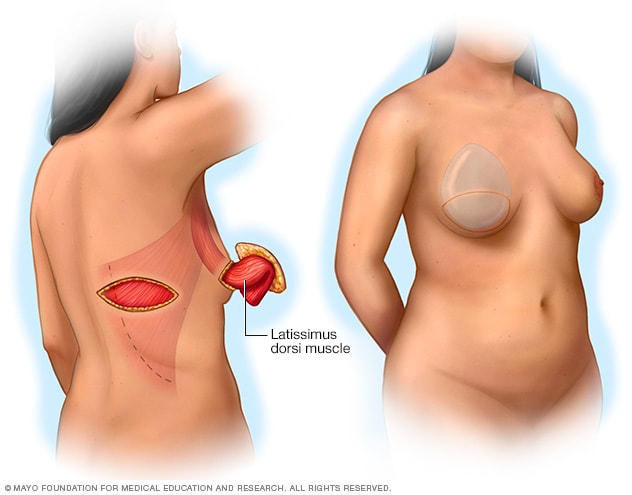 Latissimus dorsi flapOpen pop-up dialog box
Latissimus dorsi flapOpen pop-up dialog box
The tissue for reconstructing your breast most often comes from your abdomen. Tissue from your back or — less commonly — your buttocks may also be used. Your surgeon determines which method is best for you based on your body type and your medical and surgical history.
- Abdomen (TRAM flap). Your surgeon removes tissue — including muscle — from your abdomen in a procedure known as a transverse rectus abdominis muscle (TRAM) flap. The TRAM flap can be transferred as a free flap or a pedicled flap.A pedicled TRAM flap uses your whole rectus muscle — one of the four major muscles in your abdomen. For a muscle-sparing free TRAM flap, your surgeon takes only a portion of your rectus abdominis muscle, which may help you retain abdominal strength after surgery.
- Abdomen (DIEP flap). A newer procedure, deep inferior epigastric perforator (DIEP) flap, is similar to an msTRAM flap, but only skin and fat are removed. Most of the abdominal muscle is left in place and minimal muscle tissue is taken to form the new breast mound. Reattaching blood vessels requires expertise in surgery through a microscope (microsurgery).An advantage to this type of breast reconstruction is that you’ll retain more strength in your abdomen. If your surgeon can’t perform a DIEP flap procedure for anatomical reasons, he or she might opt for the msTRAM procedure instead.
- Abdomen (SIEA flap). A variation of the DIEP flap, the superficial inferior epigastric artery (SIEA) flap uses the same abdominal tissue but relies on blood vessels that aren’t as deep within the abdomen. This provides a less invasive option, but not all women’s SIEA blood vessels are adequate for this type of flap surgery.
- Back (latissimus dorsi flap). This surgical technique takes skin, fat and muscle from your upper back, tunneling it under your skin to your chest. Because the amount of skin and other tissue is generally less than in a TRAM flap surgery, this approach may be used for small and medium-sized breasts or for creating a pocket for a breast implant. Although uncommon, some women experience muscle weakness in the back, shoulder or arm after this surgery.
- Buttocks (gluteal flap). A gluteal flap is a free flap procedure that takes tissue from your buttocks and transplants it to your chest area. A gluteal flap may be an option for women who prefer tissue reconstruction but who don’t have enough extra tissue in their backs or abdomens.
- Inner thigh (TUG). Another newer option, the transverse upper gracilis (TUG) flap, uses muscle and fatty tissue from the bottom of the buttocks to the inner thigh. TUG flap surgery, which isn’t available everywhere, may be an option for women whose thighs touch and who have small to medium-sized breasts.
Because adequate blood supply is critical to the survival of transplanted tissue in flap surgery, your surgeon may prefer not to perform a pedicled flap procedure if you’re a smoker or if you have diabetes, vascular disease or a connective tissue disorder. If you smoke, you may be asked to quit for four to six weeks before your surgery. Also, obesity may preclude you from having a pedicled TRAM flap.
In general, flap breast reconstruction surgery is more extensive than is mastectomy or implant reconstruction. Flap procedures result in larger incisions that take longer to heal, so they require a longer recovery period and may require a longer hospital stay.
A new technique for breast reconstruction, autologous fat grafting, uses liposuction to gather fat tissue from your thighs, abdomen or buttocks to reconstruct the breast or to improve the appearance of your breast after reconstruction.
Nipple reconstruction
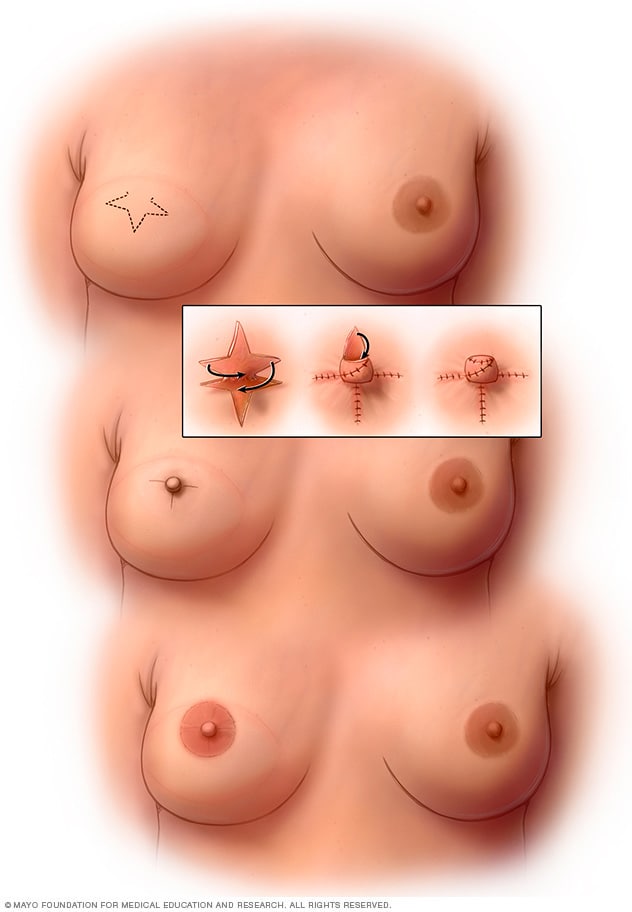 Nipple reconstructionOpen pop-up dialog box
Nipple reconstructionOpen pop-up dialog box
Breast reconstruction may also entail reconstruction of your nipple, if you choose, including tattooing to define the dark area of skin surrounding your nipple (areola).
Recovery
You may be tired and sore for a few weeks after your surgery. Your doctor can prescribe medication to control your pain. You may have drainage tubes in place for a short time after your surgery to remove excess fluids that collect in the surgical site.
Wearing an elastic bandage or support bra can help keep swelling down and support your breast while it heals.
You’ll also have stitches (sutures) after your surgery. They’ll probably be absorbable sutures, though, so you won’t need to have them removed. Scarring is permanent, but the scars generally fade over time.
Getting back to normal activities may take up to six weeks or more. Your doctor will let you know of any restrictions to your activities, such as avoiding overhead lifting or strenuous physical activities. Don’t be surprised if it seems to take a long time to bounce back from surgery — some women report that it takes as long as a year or two before feeling completely healed and back to normal.
Future breast cancer screening
If you’ve had only one breast reconstructed, you’ll need to have screening mammography done regularly on your other breast. Mammography isn’t necessary on breasts that have been reconstructed.
You may also choose to perform breast self-exams on your natural breast and the skin and surrounding area of your reconstructed breast. This may help you become familiar with the changes to your breast after surgery so that you can be alert to any new changes and report those to your doctor.
Results
Keep your expectations realistic about your surgery. Breast reconstruction offers many benefits, but it won’t make your breast look or feel exactly like it did before your mastectomy.
What breast reconstruction can do:
- Give you a breast contour
- Help your breasts look natural under clothing or a bathing suit
- Help you avoid the need for using a form (external prosthesis) inside your bra
What breast reconstruction might do:
- Improve your self-esteem and body image
- Partially erase the physical reminders of your disease
- Require additional surgery to correct reconstructive problems
What breast reconstruction won’t do:
- Make you look exactly the same as before
- Give your reconstructed breast the same sensations as your normal breast