After radiation therapy, there are many options for breast reconstruction. Whether your choice is an implant or autologous tissue reconstruction, you should discuss it with your plastic surgeon. He or she can guide you through the process and make recommendations based on your individual needs and desires.
In this guide, we review the aspects of Breast Implant After Radiation, how to prevent capsular contracture after radiation, implants after lumpectomy radiation treatment, and problems with breast implants after mastectomy.
Breast Implant After Radiation
If you’ve recently been diagnosed with breast cancer or are being treated for it, it may be difficult to think about your future. You’re probably concerned about the physical changes that will happen as a result of treatment, but there’s another aspect to consider: how your life will change. One major change is that reconstruction surgery after mastectomy is now more common than ever before. In this article, we’ll go into detail about the timing and options for reconstructive surgery after radiation therapy for breast cancer patients.
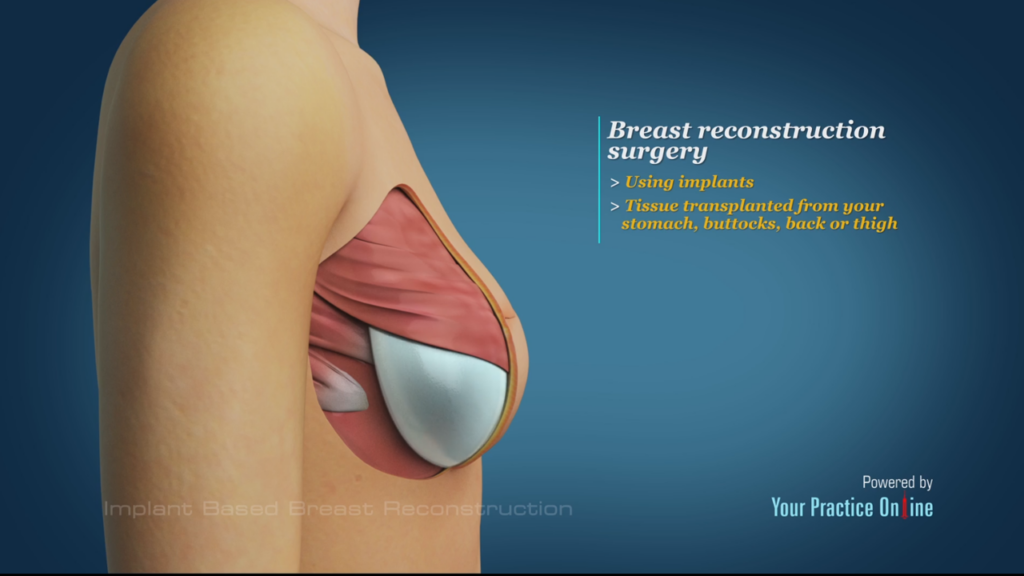
Reconstruction with an implant after radiation
Radiation therapy can damage the skin, fat and muscle tissue, nerves, blood vessels and breast tissue. The radiation oncologist will work with your plastic surgeon to create a reconstruction plan that suits your needs. The following are some things to consider when deciding on reconstructive surgery after radiation:
- Your plastic surgeon may recommend reconstruction immediately after your breast cancer treatment is complete. Waiting longer may result in less natural-looking results due to scarring or stretch marks caused by weight gain or loss during treatment.
- Your plastic surgeon may recommend waiting until you’ve finished growing before undergoing any type of reconstruction procedure so that he or she can see what size breasts look best on you before performing any operation.
- You should discuss the pros and cons of each type of operation with both surgeons before making a decision about which one is best for you; however, only one kind (autologous tissue flap) allows for more natural-looking results than others due to its use of healthy donor skin from another area on your body (such as behind a knee).
Timing of the reconstruction
When you have a mastectomy and reconstruction with breast implants, there are two times when your body will be ready for the procedure:
- At the same time as your mastectomy; this is called immediate reconstruction. This is done because radiation can affect the healing of tissue, so it’s better to get everything done at once.
- Later on, after radiation therapy is completed but before any other cancer treatments begin; this is called delayed reconstruction. The main reason for doing this is to make sure that all cancer cells have been killed or removed by radiation before placing an implant into the area where they were treated (called an “abdomen flap”).
Autologous reconstruction after radiation
Autologous reconstruction is a breast reconstruction technique that uses the patient’s own tissue. Autologous reconstruction is used for patients who have had radiation therapy after a mastectomy.
The most frequently performed autologous technique is the DIEP flap, which involves removing fat and muscle from the abdomen and transferring it to replace tissue in the breast. A second type of autologous procedure involves placing an implant into an area on your chest wall where there’s no skin or muscle left from radiation treatment. This type of procedure allows you to use your own body fat for breast reconstruction instead of having an implant placed directly under your skin in one specific location. You may also consider using another kind of implant called Alloderm® as part of this procedure, because Alloderm® has been shown to reduce scarring during breast augmentation surgery (although it’s not currently approved by the U.S Food and Drug Administration).
Immediate implant reconstruction following mastectomy and radiation therapy
Implant reconstruction following mastectomy and radiation therapy is possible but not recommended. The risks of radiation to the implant are unknown, and likely higher in women with a history of radiation therapy. As such, this approach should be considered only for women who meet criteria for immediate breast reconstruction following mastectomy and have no history or suspicion of disease recurrence.
Using a breast implant to reconstruct breasts after radiation requires careful timing and consideration.
If you’re planning to use a breast implant to reconstruct your breasts after radiation, it’s important to consider timing. You can have the implants placed at the time of surgery (mastectomy), at the time of radiation therapy, or months later.
The timing depends on how much tissue remains after your treatments. If you have enough remaining breast tissue that won’t be destroyed by radiation, then having an implant inserted at this time is ideal because they won’t need as much slack space as they would if inserted later. The longer an implant has been in place before treatment begins, the greater its chances of being damaged by radiation and losing its shape and fullness over time due to scar tissue buildup around it.
If there isn’t enough healthy tissue left for an implant after treatment has started—or if there were no options for reconstruction surgery—then a reconstruction may not be possible until after all treatments are finished (including chemotherapy). In this case, there are still options available!
A surgeon can insert temporary saline implants during surgery so that when recovery from cancer treatment is complete (and hopefully new skin cells grow back), she can then remove these temporary saline devices from underneath her skin and replace them with permanent silicone devices like those used in cosmetic breast augmentation surgeries.”
how to prevent capsular contracture after radiation
No matter how skilled your surgeon, or how perfectly your breast augmentation procedure goes, there is a small risk of complications arising during or after surgery. Every body responds differently to surgery and the insertion of a foreign object. From patient to patient, the connective tissue composition can vary widely, and no two healing processes are identical.
Some people naturally develop thick scar tissue after any kind of skin injury, while others can undergo deep cuts and only develop subtle scarring that gradually fades. Another prime example of this difference is how some women develop stretch marks after pregnancy, no matter how hard they work to prevent them, while others have babies stretch mark-free. Add to this equation our immune system responses, and you get the complex equation that determines how the body handles breast augmentation recovery.
Nowadays, medical advances, along with increased surgical skill and understanding, have made complications after plastic surgery rare. Today, we can predict which patients may be likely to experience issues with great accuracy.
If you are prone to thick scar tissue, your doctor may advise against invasive procedures, or use special surgical techniques to keep scarring out of sight. Still, one of the most common concerns we hear about from patients is capsular contracture. Below, we’ll break down what this condition is, and the techniques we can employ to lower your risk even more.
What Is Capsular Contracture?
During the post-implant healing process – whether the implant is cosmetic or medical – the body’s development of a scar tissue “capsule” around the device is a normal and crucial part of recovery. It’s the body’s automatic reaction to a foreign object, creating a barrier around it. With breast implants, this is usually for the best, helping the implant stay in place and prevent slippage.
However, in some patients, the scar tissue capsule becomes abnormally hard and can begin to contract around your implant(s). In early stages, this can cause aesthetic problems and, in untreated or extreme instances, pain in the breasts. Research has shown that around one-sixth of breast implant patients experience some form of capsular contracture, though symptoms may not always be obvious.
In most cases, capsular contracture happens sometime during the initial healing process. Around 75% of all capsular contractures occur within two years of implant placement. Rarely, this condition can occur several years after your augmentation. If it occurs at any time, contact your doctor as soon as possible to receive treatment and check for implant ruptures.
3 Techniques to Reduce Your Risk
Though it’s impossible to eliminate the risk of capsular contracture for every patient, plastic surgery has come a long way in reducing the dangers. To that end, Dr. Armijo employs several preventive strategies to help ensure your implants are healthy for years to come. The first step happens well before your surgery. During your initial consultation, Dr. Armijo will screen you for any health conditions that increase the risk of complications. You’ll also need to give up smoking for at least three weeks before your procedure and for the entirety of the recovery process to aid healing.
1. Choose the Right Implant Size and Type
One of the most effective methods of reducing capsular contracture risk is choosing the correct implant size for your anatomy. Dr. Armijo will determine what size implant your body’s natural breast tissue will adequately cover.
If you have naturally small breasts or low breast volume, we recommend increasing size in stages. That way, your body can slowly become accustomed to a mid-sized implant. After your skin stretches over time, Dr. Armijo can safely place a larger implant during a follow-up procedure.
The type of implant used can lower risks as well. Research has shown that using textured surface gel implants (rather than smooth) reduces the likelihood of capsular contracture. Doctors believe this is due to the textured surface being a bit more difficult for the body to form thick scar tissue around. However, textured implants are not right for every patient, and are best suited to submuscular placement. During your consultation, we’ll discuss all the options available and build a treatment plan to best provide the safe results you want.
2. Minimize Implant Handling
The handling of an implant before insertion into the body can increase the risk of bacterial contamination. Dr. Armijo is meticulous in strictly limiting how much he touches any implant before placing it into the breast cavity. By working with a board-certified plastic surgeon, you know you’ll receive the highest level of care and safety standards.
3. Submuscular Implant Placement
By placing your implant under the chest muscle, Dr. Armijo can significantly lower your risk of capsular contracture. If you choose completely submuscular placement, you’ll only face a 4 to 8% lifetime risk of capsular contracture. However, even if you choose over-the-muscle placement, the lifetime risk of capsular contracture is a relatively low 12 to 18%.
implants after lumpectomy radiation treatment
Implants are often a very good option for reconstructing the breast following mastectomy. However, when breast implants are placed before or after radiation therapy, there is an increased incidence of aesthetic and physical issues that arise. Potential problems can include severe hardening of scar tissue around the implant, chest wall discomfort, changes in implant position, and even implant loss.
Resultant breast implant issues can severely affect quality of life. To potentially improve adverse changes caused by radiation, autologous tissue breast reconstruction may be an excellent solution. Autologous tissue reconstruction involves transfer of excess tissue, often from the abdominal wall, to the chest to create the new breast. This involves specialized techniques of microsurgery.
Dr. Jay Orringer is a double board-certified plastic surgeon with over 30 years of breast reconstruction experience. He is also fellowship-trained in microsurgery.
How Does Radiation Affect Breast Implants?
Radiation often has serious adverse effects on both breast reconstructions and breast augmentations. The presence of a breast implant does not prevent radiation therapy from working. However, this cancer treatment can have an undesirable impact on the tissue surrounding an implant.
The body considers a breast implant a foreign object and isolates it with a barrier of protective scar tissue. This tissue, known as a capsule, is usually soft and unnoticeable. However, chest wall radiation increases the chance that the tissue capsule will harden and contract around an implant, creating a breast that is frequently tight, high in position, hard, and uncomfortable. This is a condition known as capsular contracture.
Prior radiation to the chest wall can also create unique challenges for implant-based reconstruction in the future. For example, radiation permanently adversely affects skin and underlying tissue quality. As a result, the risk of complications and poor aesthetic outcome are significantly increased following radiation.
Potential Implant Complications and Failure
Whether an implant is placed before or after radiation, the radiation will adversely affect the quality of an implant reconstruction. In addition to capsular contracture, you may experience the following breast implant problems:
Breast implants may need to be removed to remedy these issues. When this happens, it is known as a failed implant reconstruction. A failed reconstruction can be devastating, especially if subsequent implant-based reconstructions continue to produce less than optimal results.
Post-Radiation Breast Reconstruction Challenges
While the intensity of the radiation effects may decrease with time, the changes are still permanent and can make certain reconstruction approaches challenging. Attempting to satisfactorily expand the scarred post-radiation tissues is often not possible.
Similarly, placing an implant to fill a post-radiation defect is often ineffective because the scarring is most severe at the site of the previous tumor. The implant may fill the breast everywhere but where you need it the most.
Autologous Tissue Reconstruction after Radiation
In some circumstances, post-radiation implant results may be satisfactory, particularly in the shorter term. However, when implant-based reconstruction fails or creates an undesirable result, autologous tissue reconstruction can potentially offer you a much more natural, comfortable, and long-term outcome.
Excess skin and fat can be transferred usually from the abdomen (DIEP flap), buttocks (SGAP flap), or back (TDAP flap). Unlike an implant, these autologous tissue flap options, taken from another part of the body, bring in their own blood supply and may improve the quality of the radiated chest wall tissues. Blood vessels are reconnected under the microscope to complete the transplant of healthy tissue. The donor site, particularly when the abdomen is used, may have a nicely improved contour.
If you are experiencing ongoing aesthetic issues or implant complications due to radiation or other factors, autologous tissue reconstruction may be appropriate for you. Dr. Orringer will take the time to understand your unique situation to determine if autologous tissue reconstruction might meet your needs.
Schedule Your Beverly Hills Consultation
Please contact us to schedule your caring and individualized consultation with Dr. Orringer today. He will be happy to discuss your options for potentially correcting failed or unsatisfactory implant reconstructions due to radiation or other causes. We proudly welcome patients from Beverly Hills, Los Angeles, Santa Monica, Hollywood, Newport Beach, and Northern California, as well as nationally and internationally.
problems with breast implants after mastectomy
Implants are often a very good option for reconstructing the breast following mastectomy. However, when breast implants are placed before or after radiation therapy, there is an increased incidence of aesthetic and physical issues that arise. Potential problems can include severe hardening of scar tissue around the implant, chest wall discomfort, changes in implant position, and even implant loss.
Resultant breast implant issues can severely affect quality of life. To potentially improve adverse changes caused by radiation, autologous tissue breast reconstruction may be an excellent solution. Autologous tissue reconstruction involves transfer of excess tissue, often from the abdominal wall, to the chest to create the new breast. This involves specialized techniques of microsurgery.
Dr. Jay Orringer is a double board-certified plastic surgeon with over 30 years of breast reconstruction experience. He is also fellowship-trained in microsurgery.
How Does Radiation Affect Breast Implants?
Radiation often has serious adverse effects on both breast reconstructions and breast augmentations. The presence of a breast implant does not prevent radiation therapy from working. However, this cancer treatment can have an undesirable impact on the tissue surrounding an implant.
The body considers a breast implant a foreign object and isolates it with a barrier of protective scar tissue. This tissue, known as a capsule, is usually soft and unnoticeable. However, chest wall radiation increases the chance that the tissue capsule will harden and contract around an implant, creating a breast that is frequently tight, high in position, hard, and uncomfortable. This is a condition known as capsular contracture.
Prior radiation to the chest wall can also create unique challenges for implant-based reconstruction in the future. For example, radiation permanently adversely affects skin and underlying tissue quality. As a result, the risk of complications and poor aesthetic outcome are significantly increased following radiation.
Potential Implant Complications and Failure
Whether an implant is placed before or after radiation, the radiation will adversely affect the quality of an implant reconstruction. In addition to capsular contracture, you may experience the following breast implant problems:
Breast implants may need to be removed to remedy these issues. When this happens, it is known as a failed implant reconstruction. A failed reconstruction can be devastating, especially if subsequent implant-based reconstructions continue to produce less than optimal results.
Post-Radiation Breast Reconstruction Challenges
While the intensity of the radiation effects may decrease with time, the changes are still permanent and can make certain reconstruction approaches challenging. Attempting to satisfactorily expand the scarred post-radiation tissues is often not possible.
Similarly, placing an implant to fill a post-radiation defect is often ineffective because the scarring is most severe at the site of the previous tumor. The implant may fill the breast everywhere but where you need it the most.
Autologous Tissue Reconstruction after Radiation
In some circumstances, post-radiation implant results may be satisfactory, particularly in the shorter term. However, when implant-based reconstruction fails or creates an undesirable result, autologous tissue reconstruction can potentially offer you a much more natural, comfortable, and long-term outcome.
Excess skin and fat can be transferred usually from the abdomen (DIEP flap), buttocks (SGAP flap), or back (TDAP flap). Unlike an implant, these autologous tissue flap options, taken from another part of the body, bring in their own blood supply and may improve the quality of the radiated chest wall tissues. Blood vessels are reconnected under the microscope to complete the transplant of healthy tissue. The donor site, particularly when the abdomen is used, may have a nicely improved contour.
If you are experiencing ongoing aesthetic issues or implant complications due to radiation or other factors, autologous tissue reconstruction may be appropriate for you. Dr. Orringer will take the time to understand your unique situation to determine if autologous tissue reconstruction might meet your needs.
Schedule Your Beverly Hills Consultation
Please contact us to schedule your caring and individualized consultation with Dr. Orringer today. He will be happy to discuss your options for potentially correcting failed or unsatisfactory implant reconstructions due to radiation or other causes. We proudly welcome patients from Beverly Hills, Los Angeles, Santa Monica, Hollywood, Newport Beach, and Northern California, as well as nationally and internationally.
